Psoriasis
Alleviate the Symptoms of Psoriasis with our Proven Treatments at Dermatology Office, P.C.!
If you are one of the estimated two to three percent of the U.S. population that has Psoriasis, then the raised, red, scaly patches that develop on your skin can cause self-consciousness. At Dermatology Office, P.C., we specialize in the treatment of a wide range of chronic skin conditions, including psoriasis.
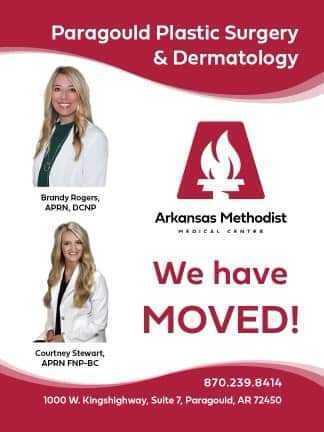
Dermatology Office, P.C., has three locations to conveniently serve you in Poplar Bluff & Dexter, Missouri and in Paragould, Arkansas. Contact us today to schedule a consultation
What Causes Psoriasis?
This autoimmune disease continues to be extensively studied, and while genetics and the immune system are both thought to play vital roles in the development of this condition, the exact cause is unknown. Although this skin condition is not contagious, it can develop at any age and affect multiple areas of the body, such as the:
- Elbows
- Knees
- Scalp
This condition may appear as a rash and can also be associated with other uncomfortable symptoms such as:
- Itching
- Burning
- Stinging
- Developing these red, scaly patches as a side effect of underlying medical conditions such as Diabetes and Heart Disease
As other types of rashes and skin irritations may be confused for this condition, it is important to have your individual condition medically diagnosed and evaluated before beginning treatment.
How is Psoriasis Treated?
The treatment of this condition may depend on its location on the body. For scalp Psoriasis, approved medications are available and have been formulated to be safe and effective for the skin. As this condition can also potentially spread to the face, back of the neck, and the ears, our medical team may suggest alternative forms of treatment in order to protect these sensitive areas.
At Dermatology Office, P.C., Dr. Yeoman and our medical team have extensive experience treating a variety of Psoriasis cases. We will provide a comprehensive evaluation of your skin and create a personalized treatment plan for your specific needs so you can feel confident about your skin.
What Triggers Psoriasis?
Although our treatments are clinically proven to control flare ups, there are other factors that can help control this condition. Studies have shown that this condition can also be triggered by:
- Stress
- Sunburns, scratches, and other skin injuries
- Certain medications
- Specific allergies, diet, and other environmental factors
Contact Dermatology Office, P.C. today to schedule your consultation with Dr. Yeoman and our medical team and have your Psoriasis treated and managed by our expert team of skin care professionals.
Find out how you can relive dry skin by following downloading our free guide today!